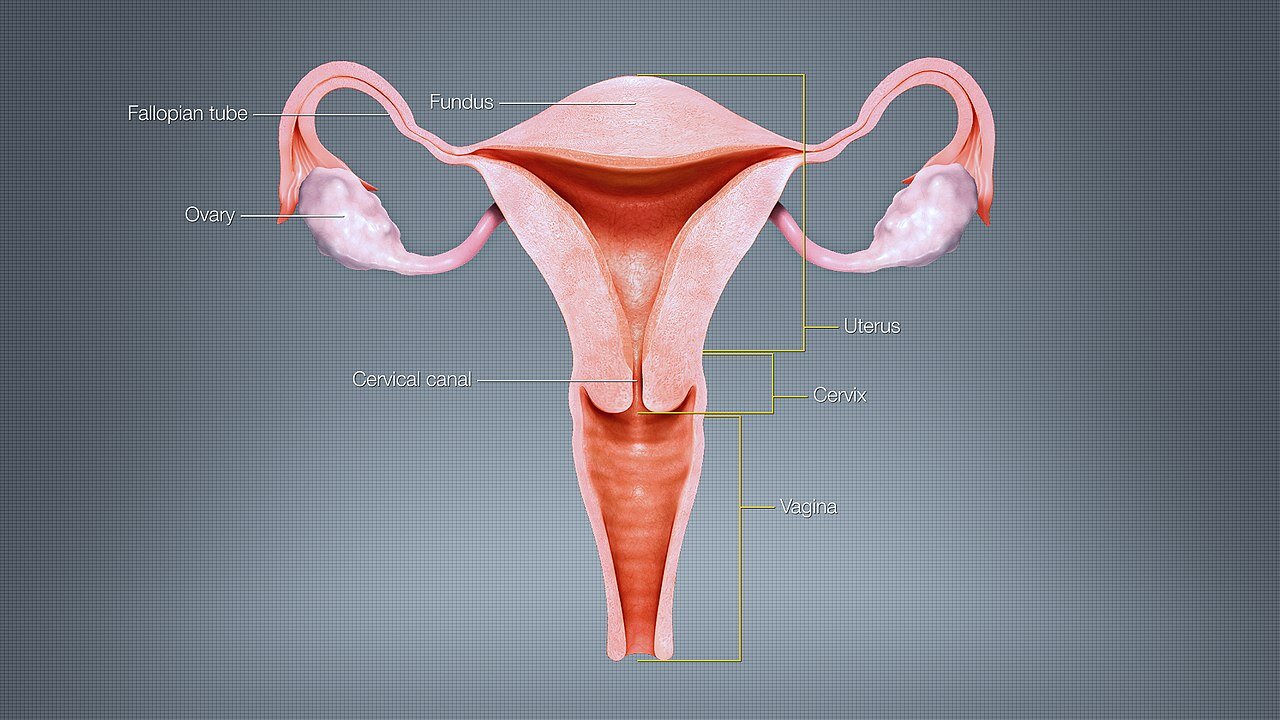
The Ins and Outs of the Female Reproductive System
Let’s get down and dirty.
Okay, before I move on, get your mind out of the gutter. I’m talking about the anatomy & physiology of the female reproductive system.
I’ve shared the basics on Instagram, and the responses were inspiring.
Hearing from women who are so eager to learn, yet know so little, about their own bodies makes me feel even more motivated to share the knowledge all women are entitled to. As women, we have this incredibly powerful reproductive system inside each of us and we should know all about it!
Below are the basics of the anatomy & physiology of the female reproductive system, compiled in one place for you as a quick reference guide.
UTERUS: the uterus is a muscular, hollow, pear-shaped organ that contains and nourishes the embryo and fetus from the time the fertilized egg implants in the uterine lining to the time of birth.
There are two main parts of the uterus:
1. Body: the uterine body has distensible walls that expand during pregnancy. The fundus, the rounded, uppermost part of the uterus, has strong muscular walls that contract during labor and childbirth.
The uterine wall is composed of three distinct layers:
Peritoneum: the outer layer
Myometrium: the middle layer
Endometrium: the inner layer that undergoes proliferative and secretory changes during the menstrual cycle
2. Cervix: lower part of the uterus that joins the vagina
CERVIX: the cervix consists of an internal os, cervical canal, and external os.
The cervical epithelium, or lining, accumulates cervical mucus rich in protein in response to the hormone called estradiol.
Cervical mucus functions as a hormone-dependent barrier for sperm to enter the uterus. Basically, it is the decision of the cervical mucus if it wants to let sperm enter the uterus and make its way to the fallopian tubes to fertilize an egg.
At mid-cycle, estrogen levels are high due to the development of a dominant follicle to be ovulated that month. The elevated estrogen levels cause the cervical mucus to become clear, thin, and highly elastic, and therefore, permeable to sperm. While in this state, the cervical mucus has the ability to reject poor-quality sperm so only a minority of ejaculated sperm actually enters the cervix.
Once ovulation occurs, progesterone levels peak and cause the cervical mucus to become viscous, cloudy, and impermeable to sperm, preventing sperm migration and maturation.
VAGINA: the vagina has three main functions: intercourse, menses, and birth passageway.
Vaginal mucus responds to hormones, including estradiol that promotes the growth of the uterine lining.
OVARIES: the ovaries are two-small almond-shaped organs located on either side of the uterus. The ovaries’ primary function is to store, develop, and release oocytes (eggs). Inside each ovary, a mass of cells called the corpus luteum forms after ovulation and produces progesterone.
The main body of the ovary, or cortex, is divided into an outer cortex and an inner medulla. The cortex contains numerous ovarian follicles in various stages of development. Each of the follicles contains an oocyte (egg). The medulla is connective tissue with blood vessels, lymphatic vessels, and nerve fibers.
FALLOPIAN TUBES: the fallopian tubes, also referred to as oviducts, are narrow passageways along which the oocyte (egg) travels from each ovary to the uterus.
There are two main functions of the fallopian tubes:
1. Transport: the released (ovulated) oocyte (egg) is guided into the uterus by a fringe of tissue called fimbriae lining the fallopian tubes.
2. Fertilization: fertilization occurs inside the fallopian tube. Once fertilization takes place between the sperm and the egg, this newly fertilized cell is called a zygote.
Welp, there you have it, a quick snapshot of the anatomy & physiology of the female reproductive system. My goal in providing this information is to empower you with knowledge about the reproductive system inside your body. Armed with this understanding of how your body should work, become an advocate for yourself and your future family. If your body does not seem to be functioning as it should, reach out to a specialist sooner rather than later. Now is the time to take control of your fertility.